Monkeypox
What is monkeypox?
Monkeypox is an infectious disease. The disease is a zoonosis, where the causative agent is transmitted to humans from animals. Monkeypox was first discovered in monkeys from which it transferred to humans. Monkeypox resembles smallpox, but is less infectious and, while similar, symptoms are less severe.
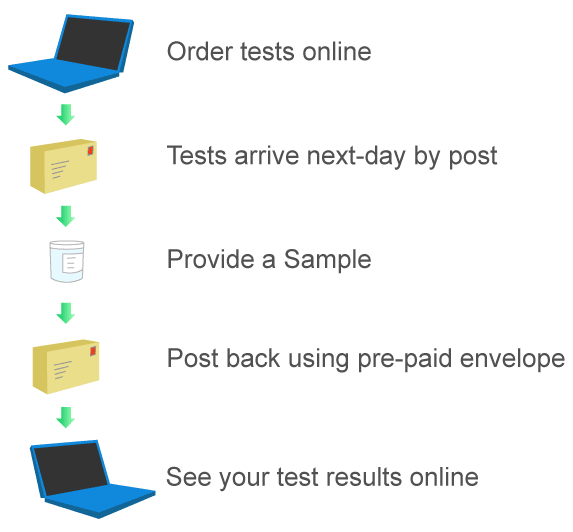
How Our Service Works
- Order your
STI test online
- Discreet package
arrives next day
- Provide a sample and post in pre-paid envelope
- Access results online
How common is monkeypox?
The first case of monkeypox in humans was in central Africa in 1970, from where it has spread to other African countries and more recently to countries outside Africa. Monkeypox is rare in the UK. On 4 August 2022, there were 2,768 confirmed cases and 91 highly likely cases of Monkey pox in the UK. The large majority of these cases are in England, particularly in London.
What causes monkeypox?
Monkeypox is caused by the monkeypox virus and is closely related to the smallpox virus.
Is monkeypox contagious?
Monkeypox is catching. Generally, monkeypox is transmitted when a person comes into close contact with an infected animal or human, or fabrics contaminated with the virus. The monkeypox virus enters the body through broken skin, mucous membranes such as the lining of the nose, mouth and eyes, and the respiratory tract.
It is thought that rodents such as squirrels, rats and mice are the main animal source of spread to humans, although monkeypox has not been found in animals in the UK. However, in central and west Africa, monkeypox can be caught from infected animals through bites and touching the animal's fur, skin, body fluids, blisters, spots, and scabs, as well as eating infected, undercooked meat.
Monkeypox spreads from person to person, but catching the virus is not easy and is uncommon. Spread between people may occur through direct contact with monkeypox skin spots/blisters/scabs (e.g., when holding hands, cuddling, and during sexual activities; it is not thought to be a sexually transmitted disease, but can be passed via sexual contact); contact with clothing or linen (e.g., towels or bed sheets/pillows) used by an infected person; and through respiratory droplets expelled by a person with monkeypox when coughing/sneezing up close to another person.
People who have been in close contact with an infected person should isolate at home for 21 days. Those who test positive for monkeypox need to isolate until they do not have symptoms and until the last scab has fallen off. Usually, symptoms are mild and people recover in 2-4 weeks, but severe cases may need to stay in hospital.
Who is most at risk of monkeypox?
Although the risk of catching monkeypox in the UK is low, anyone can catch the disease. However, many of the monkeypox cases in the West have been among men who have sex with men.
What are the signs and symptoms of monkeypox?
From the time of contact with an infected person, it usually takes from 5 to 21 days for the symptoms to start appearing. From 1 to 5 days after contact with an infected person, symptoms include fever, headache, muscle and back aches, extreme tiredness, chills, and swollen lymph nodes (glands that fight infection). A rash develops 1 to 5 days after the appearance of the first symptoms (usually a fever). The rash often starts on the face and then spreads to other areas of the body; it occurs mostly on the face, hands and feet, but the mouth, genitals, anus, and eyes may also be affected. People with monkeypox symptoms can infect other people.
The rash goes through several different stages. It starts as flat lesions (macules), which progress to slightly raised lesions (papules), then clear fluid-filled blisters (vesicles), and then yellow fluid-filled blisters (pustules). The pustules dry up to form scabs that eventually fall off. The number and size of the spots/scabs varies widely. A person is infectious until all scabs have dropped off and the skin underneath is intact. The scabs can also contain infectious monkeypox viral matter.
Symptoms usually last from 2 to 4 weeks. Some people (usually children) can develop severe disease and people with a deficient immune system may have worse outcomes. Monkeypox infections can lead to complications, such as other infections, pneumonia, and sepsis. Worldwide, death has occurred in around 3-6% of monkeypox cases.
How is monkeypox diagnosed?
Diagnosing monkeypox can be difficult as the rash can be mistaken for the rash of chickenpox. The diagnosis is confirmed following assessment by a healthcare professional and laboratory testing for the virus at a specialised laboratory. Patient information required to interpret the test results includes the dates of onset of fever and rash, specimen collection, stage of the rash, and age.
A patient self-collect test is available from The STI Clinic to do at home. The test kit is sent to you along with full instructions. Simply, a swab is used to collect a specimen from a fluid-filled lesion/blister. This is placed in a collection tube (labelled with your details), which is placed in the packing wallet for sending to the address provided as a reply paid tracked envelope. Test results are published on your patient dashboard, which only you have access to.
How is monkeypox treated?
Treatment for monkeypox mainly comprises treatment of the symptoms and management of any complications to prevent poor outcomes. Infections are usually mild and recovery generally occurs within a few weeks without treatment. However, treatment in hospital may be required in severe cases or if the person is older, a young child, or has a compromised immune system.
Only one oral medicine is licenced in Europe to treat monkeypox. This is an antiviral medicine called tecovirimat has been shown in animal studies to be effective.
Treatment is not available via this website.
When should a doctor be contacted?
You should not go to your GP clinic, hospital or a sexual health clinic if you think you may have been in contact with an infected person or have monkeypox. Instead, advice should be sought by contacting your GP, hospital or a sexual health clinic if you have a rash with blisters (especially on the face or genitals) and have, in the past 3 weeks, been in close or sexual contact with a person who has or might have monkeypox, had new sexual partner(s), or been to central or west Africa.
How can I reduce the risk of monkeypox?
You are unlikely to catch monkeypox if you have not been in very close contact with anyone with and/or has symptoms of the infection, or have not travelled to central or west Africa.
You can lower the risk of catching monkeypox by washing hands regularly or using an alcohol-based hand sanitisers; asking any sex partners, especially new partners, about their sexual health and any possible monkeypox symptoms; not having close contact with people with the infection; and not sharing towels and bed linen with people who may have monkeypox. If travelling in central or west Africa, avoid wild, stray, unwell and dead animals or touching/eating wild animal meat.
If you have monkeypox symptoms, you can lower the risk of spreading monkeypox by not having close and sexual contact until being told by a healthcare professional that you are no longer at risk of infecting other people.